Rotablation: Advancing Cardiac Care
- Dr. Srinivasa Prasad B V
- Nov 5, 2025
- 4 min read
Cardiovascular disease remains a leading cause of morbidity and mortality worldwide. Among the many challenges in treating coronary artery disease is the presence of heavily calcified plaques that resist conventional interventions. The rotational atherectomy procedure has emerged as a valuable tool in managing these complex cases. This technique allows cardiologists to safely and effectively modify calcified lesions, improving blood flow and patient outcomes.
Understanding the Rotational Atherectomy Procedure
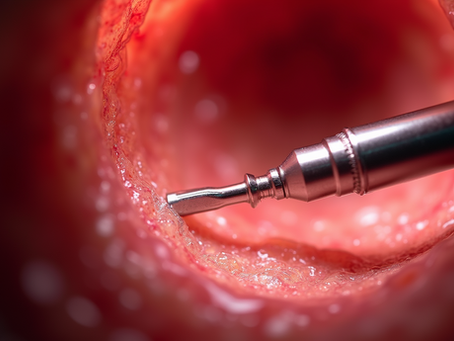
The rotational atherectomy procedure is a minimally invasive technique designed to treat calcified coronary artery blockages. It involves the use of a specialized catheter with a diamond-coated burr that rotates at high speeds. This burr sands down the calcified plaque, creating a smoother vessel surface and facilitating the placement of stents or balloon angioplasty.
This procedure is particularly useful when traditional angioplasty methods are insufficient due to the hardness and thickness of the calcified deposits. By modifying the plaque, the rotational atherectomy procedure reduces the risk of complications such as stent under-expansion or vessel dissection.
How the Procedure Works
Access and Preparation: The cardiologist gains access to the coronary artery through a small incision, usually in the wrist or groin.
Insertion of the Rotational Atherectomy Device: The catheter with the rotating burr is carefully guided to the site of the blockage.
Plaque Modification: The burr spins at speeds up to 160,000 revolutions per minute, selectively ablating the calcified plaque while sparing healthy tissue.
Post-Atherectomy Treatment: After plaque modification, balloon angioplasty or stent placement is performed to restore optimal blood flow.
This approach allows for better stent expansion and reduces the likelihood of restenosis, which is the re-narrowing of the artery.

Indications and Benefits of the Rotational Atherectomy Procedure
The rotational atherectomy procedure is indicated primarily for patients with severe calcified coronary artery disease that cannot be adequately treated with standard angioplasty. It is especially beneficial in the following scenarios:
Heavily calcified lesions that prevent balloon expansion.
Chronic total occlusions where calcification complicates crossing the blockage.
Stent under-expansion due to rigid plaque.
Lesions in small or tortuous vessels where other devices may not be effective.
Advantages of the Procedure
Improved procedural success: By modifying the plaque, the procedure facilitates stent delivery and expansion.
Reduced risk of complications: The selective ablation minimizes damage to healthy vessel walls.
Enhanced long-term outcomes: Patients experience better blood flow and reduced rates of restenosis.
Minimally invasive: The procedure is performed through small incisions, leading to quicker recovery times.
The rotational atherectomy procedure is a valuable addition to the interventional cardiologist’s toolkit, offering a solution for complex cases that were once considered untreatable.
The Role of Rotablation in Modern Cardiology
Rotablation is a term often used interchangeably with rotational atherectomy. It represents a significant advancement in cardiac care by enabling the treatment of calcified coronary lesions that pose challenges to conventional methods.
This technique has evolved over the years with improvements in device technology and procedural protocols. Modern rotablation systems offer enhanced safety features, such as controlled burr speed and improved catheter flexibility, which contribute to better patient outcomes.
Clinical Evidence Supporting Rotablation
Numerous studies have demonstrated the efficacy and safety of rotablation in complex coronary interventions. For example:
Patients with heavily calcified lesions treated with rotablation show higher rates of successful stent deployment.
The procedure reduces the incidence of major adverse cardiac events compared to balloon angioplasty alone in calcified vessels.
Rotablation facilitates the treatment of lesions in challenging anatomical locations, such as bifurcations and ostial segments.
These findings underscore the importance of rotablation as a specialized technique in interventional cardiology.

Preparing for the Rotational Atherectomy Procedure
Preparation is critical to the success of the rotational atherectomy procedure. Patients undergo a thorough evaluation to assess the extent of coronary artery disease and suitability for the procedure.
Pre-Procedure Assessment
Diagnostic Imaging: Coronary angiography and intravascular ultrasound (IVUS) or optical coherence tomography (OCT) help visualize the calcified lesions.
Medical History Review: Identifying comorbidities such as diabetes, kidney disease, or bleeding disorders.
Medication Management: Adjusting anticoagulants and antiplatelet agents to minimize bleeding risk.
Patient Counseling: Explaining the procedure, potential risks, and expected outcomes to ensure informed consent.
Procedural Considerations
Device Selection: Choosing the appropriate burr size based on lesion characteristics.
Access Site: Deciding between radial or femoral artery access depending on patient anatomy and operator preference.
Team Coordination: Ensuring the interventional team is prepared for potential complications such as slow flow or vessel perforation.
Proper preparation enhances procedural safety and effectiveness, contributing to better patient experiences and outcomes.
Post-Procedure Care and Long-Term Management
After the rotational atherectomy procedure, patients require close monitoring and follow-up care to ensure optimal recovery and long-term success.
Immediate Post-Procedure Care
Observation: Monitoring vital signs and access site for bleeding or hematoma.
Medications: Continuing antiplatelet therapy to prevent clot formation.
Imaging: Follow-up angiography may be performed to confirm vessel patency.
Long-Term Management
Lifestyle Modifications: Encouraging heart-healthy habits such as diet, exercise, and smoking cessation.
Regular Check-Ups: Periodic cardiac evaluations to detect any recurrence of symptoms.
Medication Adherence: Maintaining prescribed therapies for blood pressure, cholesterol, and diabetes control.
Patients who adhere to these recommendations experience improved quality of life and reduced risk of future cardiac events.
Embracing Innovation in Cardiac Care
The rotational atherectomy procedure exemplifies how innovation can transform cardiac care. By addressing the challenges posed by calcified coronary lesions, this technique expands treatment options and improves patient outcomes.
Healthcare providers continue to refine procedural techniques and develop new technologies to enhance safety and efficacy. As research progresses, the role of rotational atherectomy in managing complex coronary artery disease will likely grow.
For patients facing difficult coronary blockages, the availability of advanced procedures like rotational atherectomy offers hope and reassurance. It represents a step forward in the ongoing effort to combat cardiovascular disease with precision and care.






















Comments