Discover the Benefits of Transcatheter Aortic Valve Procedures
- Dr. Srinivasa Prasad B V
- Jul 26, 2025
- 4 min read
Heart health is critical to overall wellbeing, and for many patients with aortic valve disease, the options for treatment can be overwhelming. Among these options, transcatheter aortic valve procedures, including Transcatheter Aortic Valve Replacement (TAVR), have emerged as a revolutionary alternative to traditional surgeries. In this blog post, we will explore what TAVR is, the heart valve replacement options available, its benefits, costs in India, and what the future holds for this procedure.
Heart Valve Replacement Options
When it comes to heart valve diseases, patients often face a pivotal choice: surgical intervention or non-invasive options. Heart valve replacement options typically include:
Surgical Aortic Valve Replacement (SAVR): This is the standard procedure for aortic valve replacement where the damaged valve is surgically removed and replaced with a mechanical or biological valve. This option is often recommended for younger patients who can tolerate open-heart surgery.
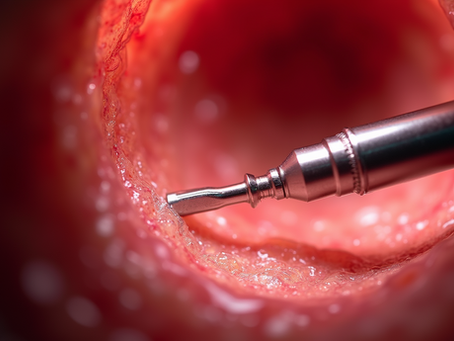
Transcatheter Aortic Valve Replacement (TAVR): This less invasive procedure is designed for high-risk patients who may not survive traditional surgery. During TAVR, a catheter is used to insert a new valve via the femoral artery, making the recovery quicker and generally less painful.
Balloon Aortic Valvuloplasty: Though not as common today, this technique involves inserting a balloon into the narrowed valve and inflating it to allow better blood flow. It's often a temporary measure until a more permanent solution can be applied.

Benefits of TAVR
Transcatheter Aortic Valve Replacement comes with a range of benefits that make it an attractive option for patients. Here’s why:
Minimally Invasive: Unlike SAVR, TAVR is performed through small incisions, leading to reduced trauma and a quicker recovery. Patients typically experience less pain and many are able to return home within a day or two post-procedure.
Lower Risk of Complications: TAVR patients often face a lower risk of complications and infections compared to those undergoing open-heart surgery.
Faster Recovery Time: Most patients can return to their normal activities within a week, a stark contrast to traditional surgery recovery that can take weeks to months.
Improved Quality of Life: Many patients experience significant improvements in their health and quality of life, including enhanced energy levels and reduced symptoms of heart disease.
Suitable for High-Risk Patients: TAVR is particularly beneficial for patients who are considered high-risk for traditional surgical procedures due to age, frailty, or other underlying conditions.

What is the Cost of TAVR in India?
Cost is an important factor when considering any medical procedure. In India, the costs for Transcatheter Aortic Valve Replacement can vary considerably depending on the hospital and the complexity of the case. On average:
The procedure can cost between INR 10,00,000 to INR 18,00,000 ($10,000 to $22,000).
The cost will typically include preoperative tests, the procedure itself, postoperative follow-ups, and medication.
It’s essential to consult with healthcare providers and insurance companies to get a clear understanding of coverage and out-of-pocket costs. Additionally, some hospitals may offer package deals inclusive of multiple services, reducing the financial burden.

What to Expect Before and After TAVR
Preparation and post-operative care play crucial roles in the success of TAVR procedures. Here’s what you can expect before and after the surgery:
Before the Procedure
Preoperative Assessment: This involves comprehensive diagnostic tests, including imaging studies, to ensure you are a suitable candidate for TAVR.
Medication Management: Patients may be required to stop certain medications, particularly blood thinners, prior to the procedure to reduce bleeding risk.
Dietary Changes: It's recommended to follow a specific diet leading up to the procedure, usually avoiding solid foods the night before.
After the Procedure
Monitoring in the Hospital: After the TAVR, patients are typically monitored for a few days to ensure their new valve is working correctly.
Cardiac Rehabilitation: Many patients benefit from cardiac rehab programs that help in recovery through monitored exercises and education on lifestyle changes.
Follow-Up Appointments: Regular follow-ups with a cardiologist are essential to assess the valve's function and any potential complications.
Future of TAVR
The future of Transcatheter Aortic Valve Replacement appears promising. Technological advances continue to improve the safety and efficacy of TAVR. Current research focuses on:
Expanded Patient Eligibility: Efforts are being made to position TAVR as a viable option for lower-risk patients, ultimately broadening its applicability.
Innovative Valve Designs: Newer and improved valve designs aim to enhance durability and performance, which could lessen the need for replacement in the future.
Hybrid Approaches: Combining TAVR with other cardiology innovations, such as different imaging technologies, may further optimize patient outcomes.
The ongoing developments in TAVR technology and procedures are expected to revolutionize cardiac care, making minimally invasive heart valve replacement more accessible for patients across different risk profiles.
In conclusion, understanding the benefits and options of transcatheter aortic valve procedures can help patients make informed decisions about their heart health. With continued advancements in technique and technology, TAVR presents a compelling option for those grappling with aortic valve disease. For more specific information and personalized advice, visit Dr. Srinivasa Prasad’s Clinic. Your heart health is valuable, and taking the time to explore your options could lead to a brighter, healthier future.


























Comments