Step-by-step guide to how the TAVI or TAVR procedure is performed
- Dr. Srinivasa Prasad B V
- Nov 6, 2023
- 2 min read
Here is a step-by-step guide to how the Transcatheter Aortic Valve Replacement (TAVR) procedure is typically performed:
Also known as Transcatheter AOrtic Valve Implantation (TAVI)
Step 1: Pre-Procedure Assessment Before the procedure, the patient undergoes a thorough evaluation, including imaging studies (such as echocardiography, CT scans, or angiography) to assess the anatomy of the aortic valve and surrounding structures.
Step 2: Anesthesia The patient is taken into the catheterization lab and placed under anesthesia. The type of anesthesia can vary and may include general anesthesia or conscious sedation, depending on the patient's condition and the preference of the medical team.
Step 3: Access Site Preparation A vascular access site is chosen, typically the femoral artery in the groin. The chosen site is sterilized, and a local anesthetic is administered to numb the area.
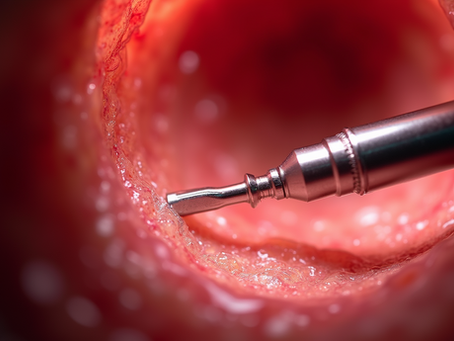
Step 4: Guidewire Insertion Using fluoroscopic guidance (real-time X-ray imaging), a thin, flexible guidewire is inserted through a needle and threaded up through the arterial system to reach the heart.
Step 5: Arterial Sheath Placement Over the guidewire, a larger sheath is inserted into the artery. This sheath provides a conduit for the delivery of the valve and other catheter-based tools to the heart.
Step 6: Catheter Delivery of Valve A specialized delivery catheter, which contains the folded replacement valve, is guided through the arterial system and into the heart using the guidewire. The catheter is carefully positioned at the site of the diseased aortic valve.
Step 7: Valve Deployment Once in position, the replacement valve is deployed. There are two main types of TAVR or TAVI valves: balloon-expandable and self-expandable.
Balloon-Expandable Valve: This type of valve is compressed around a balloon. Once it is in place, the balloon is inflated, which expands the valve and secures it in position.
Self-Expandable Valve: This valve is constructed with a stent-like frame that, once released from the catheter, expands on its own to fit securely within the native valve.
Step 8: Valve Assessment After deployment, the position and function of the new valve are assessed using various imaging techniques, such as fluoroscopy and echocardiography, to ensure it is properly seated and functioning.
Step 9: Closure of Access Site Once the valve is confirmed to be in the correct position and functioning properly, the arterial sheath is removed, and the access site in the groin is closed. This may be done using a closure device or manually by applying pressure.
Step 10: Post-Procedure Care and Monitoring The patient is monitored closely in a ICU for a period of time to ensure stability. Vital signs, including blood pressure and heart rate, are closely monitored. Once stable, the patient may be transferred to a regular room for further recovery.
It's important to note that while this is a general overview of the TAVR or TAVI procedure, individual cases may vary based on the patient's specific anatomy and medical condition. The procedure is typically performed by a team of interventional cardiologists, cardiac surgeons, and specialized nurses in a cardiac catheterization laboratory.






















Comments