Failed Surgical Heart Valve ? Consider Valve-in-Valve TAVI / TMVR
- Dr. Srinivasa Prasad B V
- Jun 28, 2023
- 3 min read
"Valve in Valve" refers to a specific application of TAVI where a new valve is implanted within a previously implanted bioprosthetic valve. This approach is used when a patient has a failing bioprosthetic valve but is at high risk for another open-heart surgery. By using TAVI for valve-in-valve procedures, it is possible to replace a worn-out bioprosthetic valve without performing a full surgical intervention.

Redo Surgery Vs Valve-in-Valve TAVI/ TAVR:
The decision between redo surgery and valve-in-valve TAVI depends on several factors and should be made on a case-by-case basis. The choice of treatment depends on the patient's overall health, the condition of the previous valve, the anatomy of the aortic valve, and the expertise and experience of the medical team.
Here are some considerations for each option:
Redo Surgery:
Durability: Surgical mechanical valve replacement typically offers better long-term durability compared to bioprosthetic valves used in TAVI. If a patient is young or has a longer life expectancy, redo surgery may be preferred to ensure a longer-lasting valve replacement.
Surgical Risk: Redo surgery is an invasive procedure that requires open-heart surgery. It may carry higher risks, especially in patients who are elderly, have multiple comorbidities, or are considered high-risk for surgical complications.
Anatomical Considerations: The anatomy of the aortic valve and the surrounding structures play a role in determining the suitability for redo surgery. Some patients may have anatomical features that make redo surgery more challenging or risky.
Valve-in-Valve TAVI:
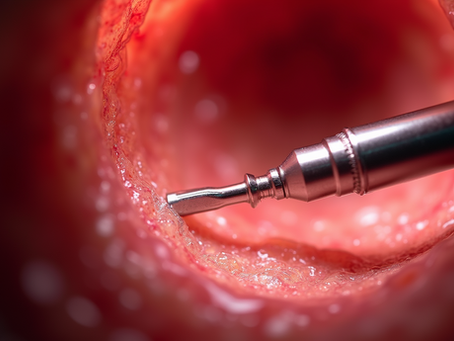
Minimally Invasive: Valve-in-valve TAVI is a minimally invasive procedure, which generally leads to shorter recovery times, reduced hospital stays, and fewer post-operative complications compared to redo surgery.
Surgical Risk: For patients who are considered high-risk or ineligible for redo surgery due to underlying health conditions, valve-in-valve TAVI can provide a less invasive alternative with lower surgical risks.
Age and Life Expectancy: Valve-in-valve TAVI may be preferred for older patients or those with shorter life expectancy, where the focus is on symptom relief and improving quality of life rather than long-term durability.
Ultimately, the decision should be made after a thorough evaluation by a multidisciplinary heart team, including cardiac surgeons and interventional cardiologists, who can assess the individual patient's situation and determine the most suitable treatment approach. The team will consider factors such as the patient's age, overall health, valve characteristics, and the risks and benefits associated with each option to provide personalized recommendations.
Risks in Valve-in Valve TAVI:
Valve-in-valve TAVI, like any medical procedure, carries certain risks. While it is generally considered a safe and effective treatment option, it's important to be aware of potential complications. Here are some of the risks associated with valve-in-valve TAVI:
Procedural risks: such as bleeding, infection, blood vessel damage, or allergic reactions to anesthesia or contrast agents. These risks are similar to those associated with the standard TAVI procedure.
Device-related risks: The implanted valve may have complications, including valve malposition, paravalvular leak (leakage around the valve), valve migration, or valve embolization (dislodgement of the valve). These issues can affect the valve's performance and may require additional interventions or surgeries.
Structural deterioration: Over time, bioprosthetic valves can degenerate and fail, regardless of whether they were implanted through surgery or TAVI. The durability of the valve-in-valve procedure depends on the condition and longevity of the original bioprosthetic valve.
Coronary artery obstruction: In rare cases, the placement of a new valve within the existing valve can obstruct the coronary arteries, which supply blood to the heart muscle. In which case, emergency coronary stenting would be required
Other complications: Other potential risks include stroke, damage to the electrical conduction system of the heart, kidney injury, or vascular complications, such as bleeding or dissection (tearing) of blood vessels.
It's important to note that the specific risks and their likelihood can vary depending on factors such as the patient's overall health, anatomy, and the skill and experience of the medical team performing the procedure. Before undergoing any medical intervention, it is crucial to have a detailed discussion with your healthcare provider, who can provide personalized information about the risks and benefits based on your specific circumstances.


























Comments